The landscape of biomanufacturing is transforming, shifting from a long-established centralized production model to a decentralized and distributed paradigm. This transition, driven by an interplay of economic pressures, environmental considerations, geographical demands, and political factors, holds potential to positively impact people’s lives globally by enabling localized, more accessible, and personalized healthcare solutions right down to the hospital level.
Historically, industrial chemical manufacturing, which includes biomanufacturing, has relied on large-scale mega-facilities that benefit from “economies of unit scale”. This traditional approach involves significant capital expenditures (CapEx), requires substantial scale, and is associated with lengthy construction times. Such a model presents high financial risk for new companies and can impede innovation by limiting industrial diversity and slowing adaptation to market changes. This production, though, can be beneficial in some cases, as unit costs decrease when output increases and fixed costs are spread over a larger volume. Furthermore, centralized facilities can restrict diversification and, as demonstrated during the COVID-19 pandemic, lead to supply chain vulnerabilities, creating calls for local manufacturing capacity for treatments like antibodies.
In contrast, decentralized biomanufacturing embraces the “economies of unit number” model, which involves the repeated production of smaller, modular units. This strategy benefits from improvements in process design gained through repetition, often described as a “learning-by-doing” approach, thereby incrementally reducing capital costs per unit capacity due to the experience curve. This shift results in that they do not depend as much on CapEx as economies of unit scale do, and there is room for improvement in both product quality and costs, either continuously or cumulatively, as the process is refined. These lower investment and financial risks not only encourage a broader and more diverse group of technology developers but also foster faster innovation and quicker responses to market demands. Moreover, this model offers greater flexibility to adapt to changing product portfolios and fluctuating demand, a critical advantage in an evolving market.
Several technological advancements are propelling this transition to decentralization. Integrated and Continuous Bioprocessing (ICB) is a key enabler, giving needed flexibility and complementing traditional batch processes with a streamlined, continuous flow. This intensifies the production process, leading to a marked reduction in facility size and operating costs; a continuous framework can shrink the facility footprint by up to 50% (Zhang 2017). End-to-end integrated continuous bioprocesses for monoclonal antibody (mAb) production have already been successfully demonstrated at pilot scale, proving the feasibility of manufacturing therapeutic antibodies with fully integrated and continuous processes (Coolbaugh 2021). The core equipment in such plants remains relatively small, yet a continuous facility built on this common framework with single-use bioreactors can rival the largest traditional fed-batch suites, capable of producing tons of material per year. This also promises improved product quality through a more uniform microenvironment throughout the manufacturing process.
The adoption of single-use technologies further facilitates decentralization. These bioreactors and mixing units, particularly prevalent in upstream and downstream processing, minimize cross-contamination and reduce the extensive needs for cleaning, sterilization, and maintenance associated with traditional stainless-steel equipment. This allows for increased plant production and supports new investment models that avoid high fixed costs. Single-use bioreactor technology enables facilities to be deployed in a modular fashion, where additional modules can be added incrementally to meet increased throughput requirements, as opposed to conventional facilities that demand full construction before production commences. This modularity also allows for staged investment, mitigating risk against an uncertain future. By enabling cost-effective use of single-use technologies, this common framework allows the fast and cheaper building of large-capacity biomanufacturing facilities in various localities.
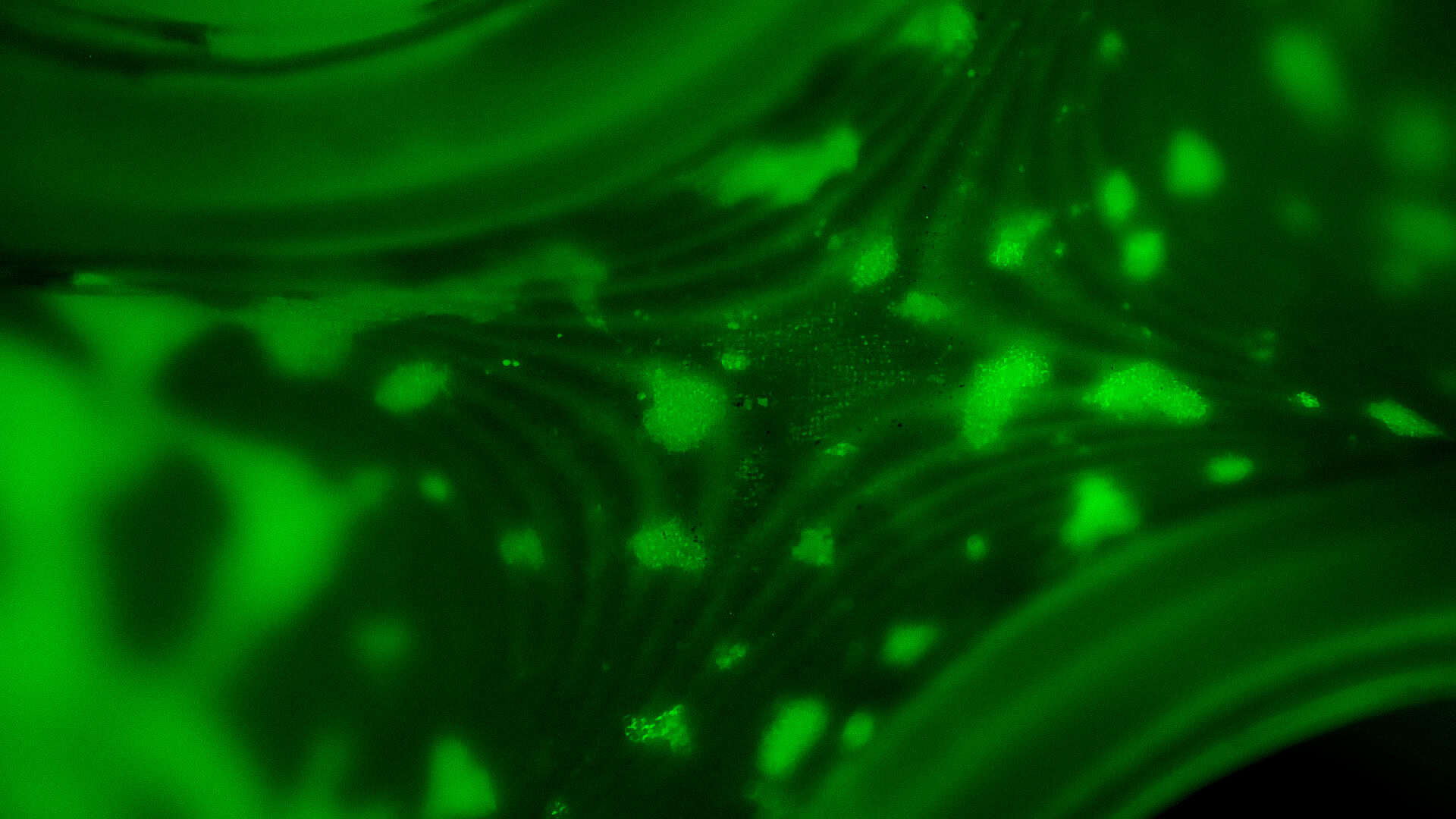
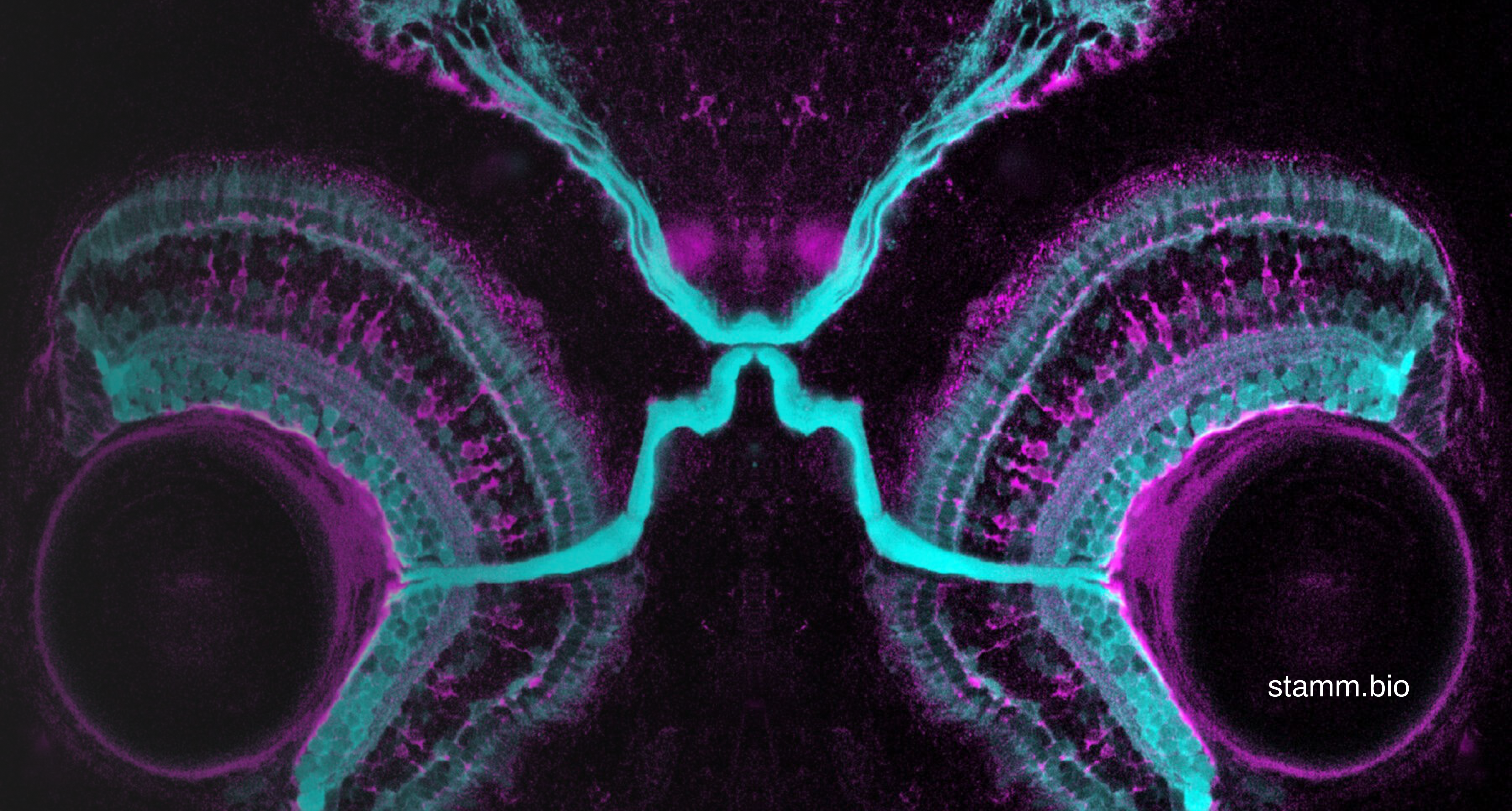
Beyond bulk production, advancements in cell and tissue engineering are contributing to the feasibility of decentralized, hospital-level biomanufacturing for personalized medicine. Regenerative medicine aims to replace, engineer, or regenerate damaged human cells, tissues, or organs, often by growing them in vitro for later implantation. Induced pluripotent stem cells (iPSCs), which can be derived from adult cells, are particularly promising as they can mitigate transplant rejection issues by being sourced from the patients themselves. The bioprocesses for manufacturing cell therapy products (CTPs), where the cells themselves are the final product, require robust infrastructure for cell harvesting, expansion, manipulation, purification, preservation, and formulation. While large-scale allogeneic therapies benefit from economies of scale, autologous therapies, derived from a patient’s cells, present logistical challenges that point-of-care technologies can address by enabling on-site product preparation in or strategically close to hospitals.
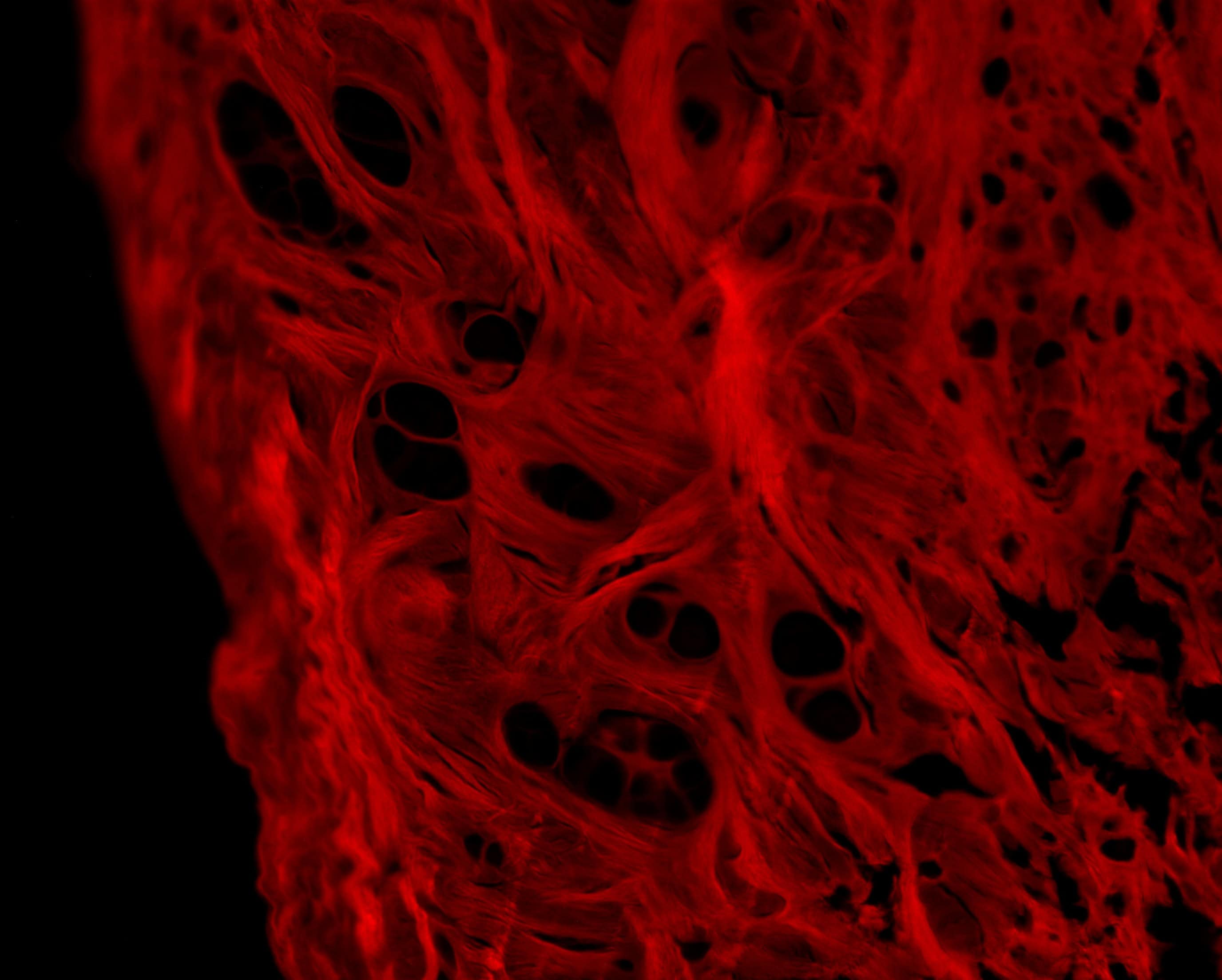
Additive manufacturing (3D printing) is a disruptive technology that directly impacts the ability to decentralize biomedical production to individual hospitals. It enables the creation of customized, patient-specific solutions with precise control over geometry, pore size, and material properties. This technology is particularly beneficial for “high-mix, low-volume” production, perfectly aligning with the needs of personalized medicine and potentially enabling manufacturing at the point-of-use. Compared to conventional fabrication methods, 3D printing offers speed and cost-effectiveness, especially for the lower production volumes typical of individual patient needs. The long-term vision includes “biofabrication” of artificial organs with vascularization and innervation, potentially performed at the site of treatment.
The positive impact on people’s lives through decentralized biomanufacturing is profound. It directly improves access to life-saving biologics, particularly in developing countries where patients and their specific treatments are often underserved. By lowering the economic barrier to chemical manufacturing, it promotes equitable resource globalization and enables countries to leverage local resources for domestic production, reducing reliance on external supply chains, as highlighted by the need for local COVID-19 treatment manufacturing. The ability of decentralized and modular facilities to be quickly expanded “at will” and with relatively low investment allows for adaptability in uncertain times, such as pandemics, or when multi-purpose facilities are required, mitigating the risk of future supply shortages.
Despite these significant advantages, the transition to decentralized biomanufacturing is not without challenges. These include navigating regulatory and practical limitations for personalized medicine due to timeframes and difficulties during clinical trials. Furthermore, the complexity of identifying the cause of deviations when products flow continuously through unit operations necessitates robust Process Analytical Technology (PAT) and sophisticated global process control strategies for real-time monitoring and adjustment. Continued advancements in biocatalyst design, process design engineering, genomic tools, and industrial automation are crucial to overcoming these hurdles and fostering this paradigm shift.
In conclusion, decentralized biomanufacturing represents a transformative leap in healthcare, serving a particular niche in accessible personalized product that slips through the industry due to the constraints of centralized mega-facilities. By leveraging innovations like integrated continuous bioprocessing, single-use technologies, and additive manufacturing, it promises to democratize access to high-quality, personalized biotherapeutics. While challenges in regulation and process control persist, the trajectory towards more distributed, flexible, and cost-effective production is clear. At Stämm, we are sure that this evolution will fundamentally enhance patient care by making essential and tailored treatments available closer to the point of need, ultimately improving health outcomes and quality of life for people worldwide.
References
Coffman, J., Brower, M., Connell‐Crowley, L., et al. (2021). A common framework for integrated and continuous biomanufacturing. Biotechnology and Bioengineering, 118(4), 1735–1749. https://doi.org/10.1002/bit.27690
Walther, J., Godawat, R., Hwang, C., Abe, Y., Sinclair, A., & Konstantinov, K. (2015). The business impact of an integrated continuous biomanufacturing platform for recombinant protein production. Journal of Biotechnology, 213, 3–12. https://doi.org/10.1016/j.jbiotec.2015.05.010
Zydney, A. L. (2015). Perspectives on integrated continuous bioprocessing—Opportunities and challenges. Current Opinion in Chemical Engineering, 10, 8–13. https://doi.org/10.1016/j.coche.2015.07.005
Kornecki, M., Schmidt, A., Lohmann, L., Huter, M., Mestmäcker, F., Klepzig, L., Mouellef, M., Zobel-Roos, S., & Strube, J. (2019). Accelerating biomanufacturing by modeling of continuous bioprocessing—Piloting case study of monoclonal antibody manufacturing. Processes, 7(8), 495. https://doi.org/10.3390/pr7080495
Coolbaugh, M. J., Varner, C. T., Vetter, T. A., et al. (2021). Pilot‐scale demonstration of an end‐to‐end integrated and continuous biomanufacturing process. Biotechnology and Bioengineering. https://doi.org/10.1002/bit.27670
Coffman, J., Bibbo, K., Brower, M., et al. (2021). The design basis for the integrated and continuous biomanufacturing framework. Biotechnology and Bioengineering, 1–11. https://doi.org/10.1002/bit.27697
Clomburg, J. M., Crumbley, A. M., & Gonzalez, R. (2017). Methane-based industrial biomanufacturing for fuel and chemical production. Science, 355, aag0804. https://doi.org/10.1126/science.aag0804
Mitsuishi, M., Cao, J., Bártolo, P., Friedrich, D., Shih, A. J., Rajurkar, K., Sugita, N., & Harada, K. (2013). Biomanufacturing. CIRP Annals – Manufacturing Technology, 62(1), 585–606 https://doi.org/10.1016/j.cirp.2013.05.001
Gottschalk, U., Brorson, K., & Shukla, A. A. (2013). Innovation in biomanufacturing: The only way forward. Pharmaceutical Bioprocessing, 1(2), 141–157
Prakash, C., Ramakrishna, S., & Pabla, B. S. (Eds.). (2019). Biomanufacturing. Springer Nature Switzerland AG. https://doi.org/10.1007/978-3-030-13951-3
Aijaz, A., Li, M., Smith, D., Parekkadan, B., et al. (2018). Biomanufacturing for clinically advanced cell therapies. Nature Biomedical Engineering. https://doi.org/10.1038/s41551-018-0246-6
Bártolo, P. J., Chua, C. K., Almeida, H. A., Chou, S. M., & Lim, A. S. C. (2009). Biomanufacturing for tissue engineering: Present and future trends. Virtual and Physical Prototyping, 4(4), 203–216. https://doi.org/10.1080/17452750903476288