In 2024, personalized medicines accounted for approximately 38% of the new drugs in development, which are targeted therapies (Personalized Medicine Coalition, 2025). Investments in R&D for precision medicine have almost doubled over the past five years, with a projected increase of 33% over the next five years. The number of precision medicines is expected to grow by 69% over the same period. (Contract Pharma, 2024). There is a clear and strong interest from many stakeholders in continuing to evolve these therapies.
What is precision medicine?
Precision medicine is an approach to medical diagnosis and treatment that, unlike the one-size-fits-all model of traditional medicine, considers the unique characteristics of each patient to create targeted therapies. This includes an individual’s lifestyle, genetic profile, and environment. The goal is to achieve more effective treatments while reducing adverse effects.
Based on the understanding that not every medication is equally effective for all patients, precision medicine integrates genetics, genomics, pharmacology, diagnostics, and prevention. As personalized medicine and related technologies become increasingly precise, we can expect a future in which disease progression is slowed, unnecessary medication is avoided, and patients’ quality of life improves, all while saving time, effort, and costs in healthcare processes.
The key aspect of precision medicine: Data.
Three main factors contribute to this acceleration:
- Computing power has grown dramatically, enabling the analysis of enormous datasets.
- Integrating diverse datasets provides deeper insights into human biology, including multiomics, biomarkers, and lifestyle and environmental factors that personalized medicine relies on.
- Advanced analytics allow researchers to connect these datasets and uncover the underlying determinants of disease.
Access to data offers substantial emerging opportunities in the field. By mining clinical datasets, researchers can identify new drug targets that might otherwise remain undiscovered. Additionally, precision medicine enables the recognition of highly responsive patient populations, creating the potential to expand targeted therapies beyond oncology into a broader range of therapeutic areas.
Also read:
Biomanufacturing 4.0: The impact of a data-driven approach.
Limits of the data
Despite these advances, limitations remain. Much of the individualized data comes from very narrow populations. Therefore, ensuring the quality, consistency, and representation of these data sets presents a significant challenge. To fully realize the promise of precision medicine, data sets must be representative of all people, not just select groups. Additionally, a small sample size can limit their statistical power.
For example, a genome-wide association study found that only 19% of the 2,500 participants in the study were of non-European descent, most of whom were of East Asian origin (Popejoy & Fullerton, 2016). This lack of representation risks linking genetic markers to diseases incorrectly and creating precision medicine for some populations while producing imprecision for others.
To address these limitations, larger and more diverse data sets are essential. Coverage across ethnic and demographic groups strengthens the predictive power of biomarkers and increases confidence in their validity.
New technologies now allow for real-time monitoring of patient physiology. While behavioral tracking devices, such as smartwatches, are currently expensive and often paid for by the user, they enable the collection of multidimensional data across diverse populations. This can improve representation in primary and secondary prevention trials and enhance predictive outcomes.
However, this approach relies heavily on patients voluntarily sharing their data. Therefore, protecting the privacy and personal information of patients is crucial to ensuring ethical handling and increasing participation in data collection initiatives.
Harnessing data at scale
Governments, research agencies, and companies have already built extensive genomic knowledge, yet much remains unknown. Progress requires Big Science approaches, understood as a “large-scale research approach that involves interdisciplinary collaboration among numerous scientists and engineers… and characterized by the use of sophisticated technologies and significant organizational structures to address complex scientific problems.” (Krige, 2001)
This is seen in population genomics programs worldwide. Today, few data sets are fully integrated across health systems. Making these investigations interoperable is critical to exponentially increase the clinical utility of these data sets and accelerate the impact of precision medicine. A robust digital infrastructure capable of supporting secure data sharing is key.
Effective use of data represents one of the greatest challenges not only in personalized medicine but across industries. In fact, in 2024, over 70 percent of surveyed healthcare organizations say that they are pursuing or have already implemented generative AI capabilities to improve organizational efficiency in this information-intensive industry (McKinsey, 2024)
Flexible manufacturing for personalized therapies
Many early-stage developments and clinical trials in personalized medicine use production approaches opposite to traditional one-size-fits-all manufacturing.
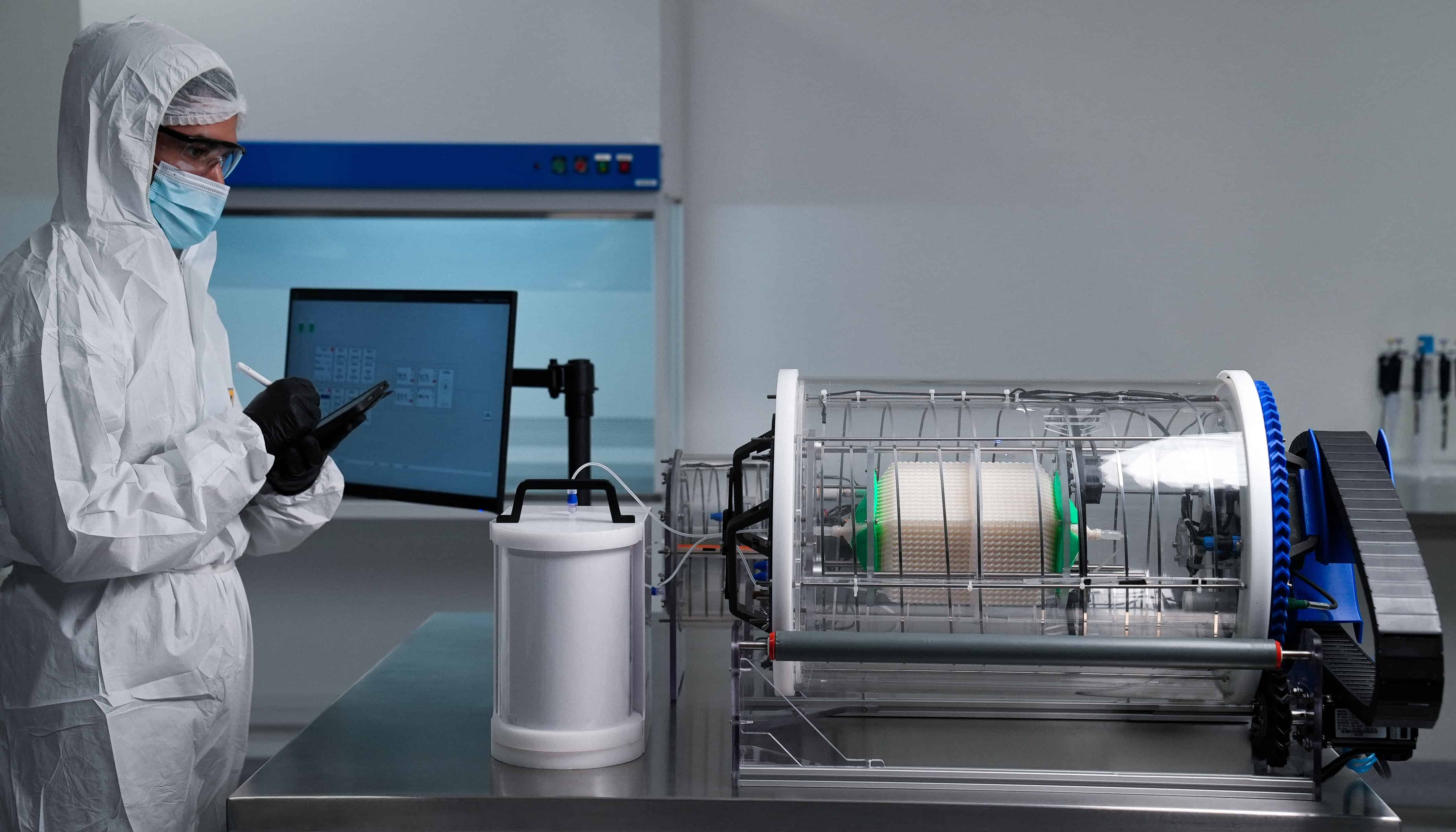
While not all personalized medicine requires single-patient production, small batches designed for patients with specific genetic attributes are increasingly common. This necessitates flexible manufacturing devices capable of rapid reconfiguration and product switching. Facilities may include multiple parallel bioreactors, producing different products simultaneously for diverse patient needs.
This patient-centric production model mimics small-scale lab manufacturing but must maintain the speed, traceability, and reliability required for safety and efficacy. Logistics also face new challenges, requiring enhanced controls to ensure precise distribution of highly specific treatments. Continuous biomanufacturing provides a solution in some scenarios, offering uninterrupted production that allows greater flexibility than traditional batch processes.
Distributed facilities reduce lead times and improve accessibility. They are particularly relevant for therapies like gene editing or CAR-T, where the patient’s own cells are part of the production process.
Read more: Revolutionizing Biomanufacturing: Building the Factory of the Future
Ensuring safety and quality in personalized medicine
Personalized approaches in medicine include approaches that change disease mechanisms (e.g., gene therapy, CRISPR) and others that target specific pathways in predefined patient groups. Regulatory focus is increasingly on manufacturing complexity and quality control, ensuring that drugs or diagnostics developed for subpopulations can move safely through clinical trials and into the market. On the diagnostic side, advanced digital analytics are required to identify patients.
Looking ahead in precision medicine
Precision medicine is transforming healthcare, driven by advances in data generation, integration, and analytics. While targeted therapies and personalized approaches are growing at unprecedented rates, significant challenges remain, including data representativeness, infrastructure, and regulatory complexity. Small-scale, flexible biomanufacturing and distributed production facilities offer solutions for producing patient-specific therapies efficiently and safely.
Looking ahead, statistics, machine learning, and artificial intelligence will play a crucial role in optimizing precision medicine. Integrating multi-omics data, leveraging real-world evidence, and applying advanced quantitative methods will improve diagnostics, treatment selection, and patient outcomes. Global collaboration and harmonized data standards will further enhance the development and accessibility of personalized therapies.
Success will depend on combining big science approaches, interoperable data sets, robust digital infrastructure, and advanced statistical tools to ensure precision medicine is not only effective but also equitable. By embracing these opportunities, healthcare can move toward truly individualized, data-driven care with improved outcomes for all populations.

Bibliography:
- Center for Devices and Radiological Health. Precision medicine. U.S. Food And Drug Administration. [Link]
- Contract Pharma. . Adapting Manufacturing for Super Small Batch, Precision Medicines. [Link]
- Krige, J. (2001). Physical Sciences: History and Sociology. En Elsevier eBooks (pp. 11418-11422). [Link]
- McKinsey&Company. (2024. Generative AI in healthcare: Adoption trends and what’s next. [Link]
- MedPath – Medical Intelligence Platform. MedPath.
- Nassar, S. F., Raddassi, K., Ubhi, B., Doktorski, J., & Abulaban, A. (2020). Precision Medicine: Steps along the Road to Combat Human Cancer. Cells, 9(9), 2056. [Link]
- New Study Illustrates Biopharmaceutical Industry’s Commitment to Personalized Medicine. (s. f.). PhRMA. [Link]
- Personalized Medicine Coalition. (2025). Personalized Medicine at FDA: the scope & Significance of progress in 2024. En Personalized Medicine Coalition.
- Popejoy, A. B., & Fullerton, S. M. (2016). Genomics is failing on diversity. Nature, 538(7624), 161-164. [Link]
- The Promise of Precision Medicine. (s. f.). [Vídeo]. [Link]
- Umulisa, K. J. (2024). Statistics in Personalized Medicine: Challenges and Innovations. [Link]